Congressional bill could reverse Medicare cuts and increase physician pay
The bipartisan bill Medicare Patient Access and Practice Stabilization Act (H.R. 879) was reintroduced in Congress to try and block the 2.83 percent Medicare pay cut physicians and actually increase the amount paid to cover inflationary costs.
If passed, this legislation would prospectively stop the 2.83% pay cut physicians received starting Jan. 1, 2025. The bill would be in effect from April 1 through Dec. 31, 2025. Compounded with the Centers for Medicare and Medicaid Services (CMS) estimates of a projected 3.6% increase in practice cost expenses for this year due to inflation, physicians could face a 6.43% cut unless Congress acts. This bill looks to reverse the payment cuts while also granting payment adjustments for inflations, for a total positive adjustment of 6.62%.
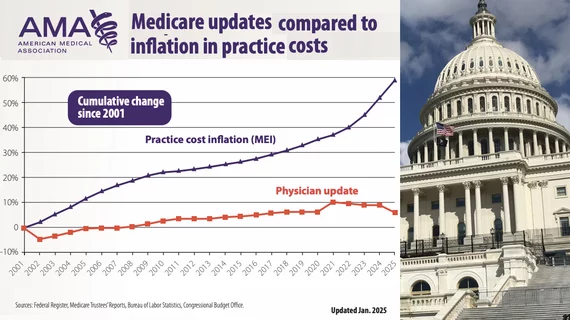
According to the American Medical Association (AMA), when adjusted for inflation, Medicare reimbursement for physician services has declined 33% from 2001 to 2025. This has spurred loud outcry from all of the major U.S. medical associations. The AMA and many societies have predicted that Medicare reimbursement cuts for physicians are creating far-reaching consequences for the American healthcare system, particularly in rural and underserved areas.
Costs for staffing and operations continue to climb, and declining reimbursement rates are forcing practices to make difficult decisions, such as layoffs, reduced services, or permanent closures. These closures are disproportionally impacting rural and lower-income areas. The AMA has said some physicians have already decided to no longer accept Medicare patients because the payments do not cover the costs for providing care.
This is also being compounded by a growing shortage of physicians and an aging population of doctors nearing retirement. These these cuts have exacerbated physician burnout and medical groups have said threaten to further limit access to care for Medicare patients.
The bipartisan bill was reintroduced Jan. 31 by Congressmen Gregory F. Murphy, MD, (R-North Carolina) a urology and renal transplantation surgeon, along with 37 co-sponsors from both sides of the aisle, including numerous physician members of the House.
"Physicians in America are facing unprecedented financial viability challenges due to continued Medicare cuts. Access to affordable and quality healthcare for millions of seniors is in severe jeopardy," said Congressman Murphy in a statement. "Doctors see Medicare patients out of compassion, not for financial gain. The cost of caring for a Medicare patient far outpaces the reimbursement that physicians receive for seeing them. On top of that, the expense of providing care continues to rise due to medical inflation. This inflation, coupled with declining reimbursement rates, creates enormous financial pressures on physicians, forcing many to retire early, stop accepting new Medicare patients, or sell out to larger, consolidated hospital systems, private equity, or even insurance companies."
Murphy said the future of private practice medicine is at stake. Policies such as Medicare awarding higher payments and inflationary increases to hospitals, but not to physicians, has led to a rapid decline in private practices. In cardiology for example, private practices employed about 90% of physicians, but that has eroded to about 12% today. He said private practices are the most cost-efficient and enable the most personalized care for patients. "This bipartisan legislation prevents further cuts, provides a modest inflationary adjustment to help ease the cost of care, and ensures Medicare remains viable for both doctors and patients," Murphy said.
"Over the past 22 years, adjusting for inflation, physicians have essentially taken a 26% pay cut from Medicare," said Congresswoman Kim Schrier, MD, (D-Washington) a pediatrician, said in a statement. "Their reimbursement has been flat or declining, while overhead costs have increased by about 47% for rent, labor, equipment and insurance. I cannot think of another profession whose compensation has dropped by 26% over two decades. Physicians have been holding their breath, year after year, hoping that Congress will act to avert these devastating decreases in reimbursement. Without adequate reimbursement, solo and small practice physicians—most often in rural or underserved areas—are already closing their doors."
March deadline approaches to reverse Medicare cuts
The AMA said the next legislative chance to reverse the Jan. 1 Medicare cuts comes in mid-March, which is the deadline for the 119th Congress to fund the federal government through the end of the fiscal year. At the end of 2024, The AMA said the 118th Congress passed a scaled-back resolution to keep the government running amid a very politically charged lame-duck session. The AMA said the language that would have stopped the physician Medicare payment cut was removed from the bill.
The AMA said it strongly supports the legislation and is working with members of Congress to meet that deadline. The group is also asking members to call their members of Congress in support of the bill, and to attend the "Fix Medicare Now” event the AMA is hosting on Capitol Hill Feb. 11, where physicians are invited to wear their white coats.
"We are using this bill...to help position ourselves in the best possible way to be in that [March] package to reverse as much of the cuts as possible and to try to get an update,” explained Jason Marino, AMA director of Congressional affairs said during a recent webinar. “We need to tell the story about the rural practice on the verge of closing because of these cuts. And they can’t afford to see Medicare patients. I’ve heard some stories from physicians that aren’t even taking a salary. They’re keeping the practice open by not taking a salary because the medical payments are going for their staff and technology. They’re not getting paid. But that’s not sustainable.”
Medical societies applaud effort to stop Medicare cuts
Medical societies responded positively to the bill and said stopping payment cuts and keeping up with inflation would go a log way to improving Medicare patient care, rather than causing frustration and forcing doctors and health systems to make tough choices.
"The Medical Group Management Association (MGMA) urges swift passage of the Medicare Patient Access and Practice Stabilization Act of 2025. Physician practices are now a month into the new year, facing uncertainty and financial shortfalls from the congressional failure to reverse the 2025 Medicare fee schedule cuts," explained Anders Gilberg, MGMA senior vice president, government affairs in a statement. "These cuts have negatively impacted the viability of their Medicare business, commercial contracts tied to Medicare rates, as well as Medicaid reimbursement in states that use Medicare as a benchmark. With nearly 80% of all physicians now employed by facilities and larger entities, Medicare beneficiaries in areas of the country that rely solely on community-based medical practices are especially vulnerable to access issues. Without immediate congressional action on this important legislation, more and more physician practices will be forced to close their doors.”
"The American Society of Nuclear Cardiology (ASNC) is urging Congress to take action, as declining reimbursement and the absence of inflationary updates pose grave challenges to physician practices,” said ASNC President Panithaya Chareonthaitawee, MD, in a statement. “According to CMS, practice costs are projected to rise 3.5 percent this year. Physicians must have increased financial stability to continue providing care to patients.”
Physician members of Congress understand the impact of Medicare cuts
The concerns shared by the AMA, MGMA and other medical associations are being echoed by several congressional co-sponsors.
"The bipartisan Medicare Patient Access and Practice Stabilization Act is crucial to reversing the damaging trend of cuts that threaten our healthcare providers, especially in underserved communities. We must act now to prevent further early retirement, burnout and consolidation," said Congresswoman Mariannette Miller-Meeks, MD, (R-Iowa) an ophthalmologist, in a statement.
"Physicians, unlike the rest of the players in healthcare, have never received an inflationary update and consistently received cuts. This bill ensures a more stable Medicare payment system, allowing providers to focus on delivering care rather than worrying about losing their practice. With this bipartisan effort, we are working toward a system that supports both doctors and patients," said Congressman Ami Bera, MD, (D-California) a doctor of internal medicine and former health system administrator, in a statement.
"After yet another cut to the physician fee schedule, more physicians will be forced to limit the number of Medicare patients they see, or in some cases, shutter their doors. This will result in a lack of access to care for many Medicare beneficiaries. While the price to administer high-quality care has continued to rise over the last 20 years, the Medicare reimbursement rate for physicians has continued to drop," explained Congressman John Joyce, MD, (R-Pennsylvania) a dermatologist, in a statement.
"Rising costs and administrative burdens make it clear that Medicare reimbursement policies must reflect the true costs of providing care," said Congressman Raul Ruiz, MD, (D-California) an an emergency room doctor, in a statement.