To nobody’s gain, psychiatric patients are getting ‘stuck’ in inpatient beds
Along with the unprecedented challenges COVID-19 has brought to U.S. hospitals in 2020 are some older sore spots that the pandemic has only inflamed.
One is an undersupply of sites in which to place psychiatric patients who are too well for inpatient care but still in need of attentive assistance to maintain their good general health.
The state of Virginia is struggling to sort out this problem within the hospitals it runs. The Roanoke Times has put faces and stories to some of the numbers.
“We are having to take care of [these patients] 24/7 and staff it as if they were in acute crisis just coming into the facility,” Alison Land, commissioner of Virginia’s mental health agency, tells the newspaper.
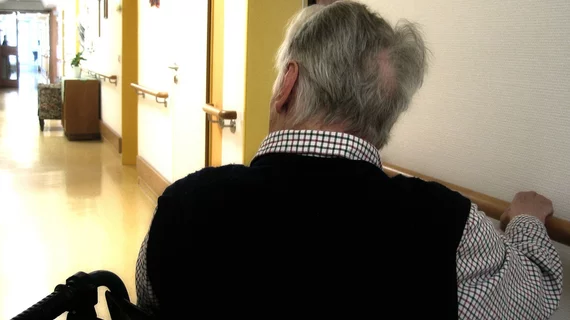
The biggest single subset of this population comprises older patients with dementia.
“They’re stuck, and we have to get them unstuck,” Land tells reporter Luanne Rife.
Rife wraps her news analysis around the story of Dennis Brown, a Virginian whose heavy drinking led to early-onset dementia in his 50s. His sister repeatedly tried to help him, but he rebuffed her attempts with first stoicism and then violence.
A series of placements in various types of facilities followed. So did more aggression and more attempts at placement, including at state-operated, 270-bed Catawba Psychiatric Hospital.
Half the beds there are reserved for older people having acute psychiatric episodes. The expectation is that they’ll be discharged to a more appropriate setting when the treatable crisis ends.
“If you can’t find a placement, that person just continues at hospital-level care. It’s expensive,” says Tamara Starnes, chief clinical officer for Blue Ridge Behavioral Healthcare. “[These patients] really could function well perhaps in a memory care setting if there was availability. So you just really get stuck in that hospital.”
And sometimes, Rife reports, people end up stuck simply because they’re in a psychiatric hospital. This carries stigma that many nursing homes prefer to avoid.
It’s unlikely the cycle is limited to Virginia. Get the rest of the story from the Roanoke Times.