Hallmark of Alzheimer’s disease detectable through AI
AI can speed up precise detection of one of the key signs of Alzheimer’s disease, according to researchers from University of California Davis and UC San Francisco, who published a study on their machine learning tool in Nature Communications.
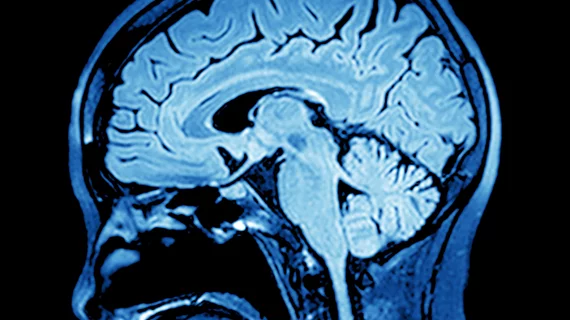
The machine learning tool developed by the researchers can detect clumps of protein fragments in the brain, called amyloid plaques, which destroy nerve cell connections and are present in people with Alzheimer’s disease. The tool works similar to how Facebook can recognize faces on captured images; it can see types of amyloid plaques very quickly in brain tissue.
Brittany N. Dugger, PhD, an assistant professor in the UC Davis Department of Pathology and Laboratory Medicine at UC Davis and lead author of the study, teamed up with Michael J. Keiser, PhD, an assistant professor in UCSF's Institute for Neurodegenerative Diseases and Department of Pharmaceutical Chemistry, to figure out if they could teach a computer to analyze and identify different types of amyloid plaques in human brain tissue. Keiser and his team designed a computer program that can recognize patterns based on thousands of human-labeled examples, called a convolutional neural network (CNN).
The CNN needed enough training examples to be able to identify the amyloid plaques on its own and train the machine learning algorithm to identify brain changes seen in Alzheimer’s disease, including seeing cored and diffuse plaques and abnormalities in blood vessels. To do this, Dugger needed to label tens of thousands of images from half a million close-up images from 43 healthy and diseased brain samples. Using a platform modeled after dating apps like Tinder, which allow users to swipe right for “yes” and left for “no,” Dugger could quickly label plaques in images at roughly 2,000 images per hour. The program was called “blob or not,” and Duggar annotated more than 70,000 blobs, or plaque candidates.
After being trained on this database, the algorithm could process a whole-brain slice slide with 98.7% accuracy. In addition, the UCSF team tested the computer’s identification skills to see why it made its predictions.
While the tool vastly outpaces humans in the ability to analyze data, it still should be considered complimentary to of an expert neuropathologist.
"We still need the pathologist,” Dugger said in a statement. "This is a tool, like a keyboard is for writing. As keyboards have aided in writing workflows, digital pathology paired with machine learning can aid with neuropathology workflows."
However, the computer could be considered better than Dugger at identifying plaques.