3 reasons humans are irreplaceable by colonoscopy AI
Despite deep learning’s 96%-plus accuracy at detecting and localizing colorectal polyps in a large recent study, gastroenterologists need not fear being replaced by machines—and patients don’t have to worry about robot colonoscopists.
The study was conducted by physicians and computer scientists at the University of California, Irvine and published in the October 2018 edition of Gastroenterology.
The commentary on it comes from GI specialists at Valduce Hospital in Como, Italy, and is current now in Translational Gastroenterology and Hepatology.
Authors Franco Radaelli, MD, and Silvia Paggi, MD, consider the study’s implications and lay out three aspects of the “human touch” without which the quality of colonoscopy procedures and interpretations would suffer significantly.
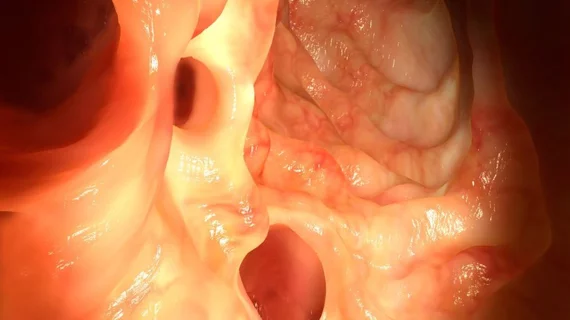
1. The skill needed to bring a polyp into the field of view. “Technique, albeit difficult to be objectively assessed, is strictly endoscopist-related and represents a powerful indicator in differentiating high and low adenoma detectors,” Radaelli and Paggi write.
2. The ability to focus attention on a lesion that is in the field of view. “Studies evaluating the impact of endoscopists’ visual gaze patterns on adenoma detection rates by using eye-tracking technology, an objective tool that detects differences in viewing patterns, [have] defined distinct visual gaze patterns that are associated with expert behavior.”
3. The capacity to differentiate a lesion of interest from the normal surrounding mucosa or other subtle mucosal lesions with no clinical relevance. “This mainly depends on the endoscopist’s experience and culture. The case of sessile serrated lesions, which have always existed but ever overlooked until recently, represents a relevant example of this situation.”
Acknowledging that the first two items in particular have more to do with the procedure than the visual inspection, Radaelli and Paggi contend that colonoscopy AI will remain dependent on human interpreters at least until AI reliably brings false-positive rates well below the 7% reported in the 2018 study.
“As demonstrated in the [UC-Irvine] study, adding new training samples not only with more polyps but also with random artifacts, such as water, air, bubbles, fecal matter and low quality blurred frames, could decrease the rate of false positive images,” they write.
Either way, they concur, “the use of computer-aided detection systems for polyp detection during colonoscopy is extremely exciting and we are sure that in the near future these technologies will be part of modern endoscopy platforms.”
Click here for the 2018 study and here for the current commentary.