MGMA: Most practice leaders unware of direct primary care
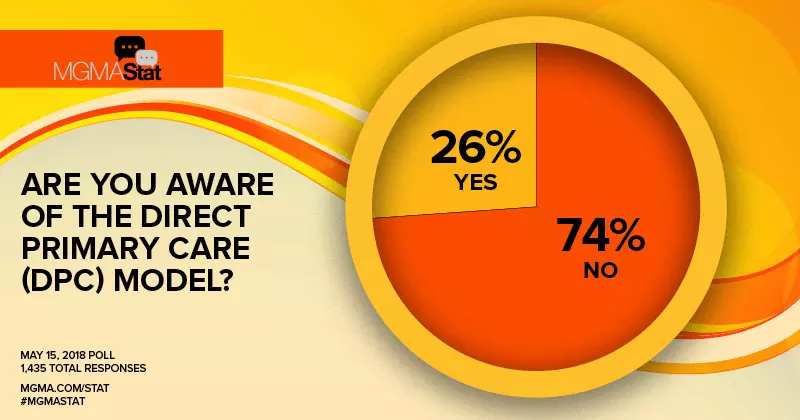
A poll conducted by the Medical Group Management Association (MGMA) found most medical practice professionals aren’t aware of the direct primary care (DPC) model where patients pay a flat fee in exchange for easier access to their primary care doctor.
The poll included 1,435 professionals responses. Within the minority who were aware of the DPC model, many respondents felt “it was convenient [and] improves cost transparency,” and they hope the model will become widely used.
Often called concierge medicine, DPC is built around patients paying a fixed fee and having most primary care services covered. Common perks for patients often include 24-hour access to physicians by phone, text or email, being able to schedule appointments the same or next day and getting more face time with doctors who aren’t being pressured to see more patients.
Proponents of the model have said it offers the improved access produces better patient outcomes, reduces administrative burden and reduces confusion about costs with its flat fee structure.
“[DPC] is a great option for docs and patients with high deductibles,” Susan Childs, president of Evolution Healthcare Consulting in Rougemont, North Carolina, said in a MGMA press release. “Doctors are choosing a lifestyle of seeing patients the way they want to.”
Versions of this model have been pushed by groups like the American Academy of Family Physicians and CMS has been collecting comments on testing a DPC-like model for Medicare beneficiaries.
Where it has been implemented, it’s also attracted controversy. Physicians at the University of Michigan’s health system criticized a new $2,700-a-year DPC program as implying that patients have to pay more in order to receive quality care and discriminates against underserved populations for the benefit of the wealthy.
“If we were a for-profit and private corporation, we could decide not to serve such patients,” Michigan Medicine doctors wrote in January. “But to imply that only the wealthy will get the best health care goes against the foundation of our training as physicians and primary care clinicians.”