‘Just Culture’ has failed to eliminate ‘culture of blame’ in hospitals
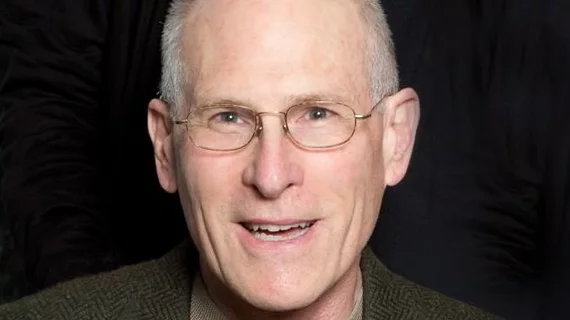
The “Just Culture” model to encourage healthcare professionals to report mistakes to focus on improving processes, not punishment, hasn’t worked, according to a study authored by Marc Edwards, MD, MBA, of the QA to QI Patient Safety Organization.
This model has been pushed for more than a decade, being adopted and endorsed by groups like the American Nurses Association and the Joint Commission. The idea is by pushing healthcare workers to report errors, adverse events and mistakes without so much fear of being blamed, organizations can learn how to improve processes. Accountability would supposedly be maintained through an algorithm separating blameless mistakes from those worthy of punishment.
Published in the American Journal of Medical Quality, the study combined data on clinical peer review practices from the Hospital Compare website with survey data from the Agency for Healthcare Research and Quality.
Edwards found out of 270 hospitals, 211 (70 percent) had adopted the Just Culture model. More than half of facilities reported it had a positive impact and only 27 percent felt it had no apparent effect. That latter group appeared to be right, as Edwards found those hospitals have shown no improvements on measures which Just Culture was meant to change: nonpunitive response to errors and frequency of events reported.
“In other words, the evidence suggests that, in aggregate, U.S. hospitals have perfected a system for casting blame among both physicians and nurses,” Edwards wrote. “In such a hostile environment, self-reporting would be career suicide. So whatever the effect of Just Culture, it clearly has not fulfilled its promise to eliminate the culture of blame and gross underreporting of opportunities for improvement, which continue to hamper progress in patient safety.”
The study did find some association between adopting Just Culture standards and having a more effective clinical peer review process.
Confusion, concern about job security and widespread variation in standards seemed to hamper hospitals’ efforts to make improvements through Just Culture. In Edwards’ follow-up discussions with participants in the study, some said viewed as a stand-alone program, others just viewed it as a set of principles to be applied to nurses and still more experienced resistance to adopting the program without understanding its goals.
“For example, in one hospital, union leaders thought that Just Culture would likely increase adverse employment decisions,” Edwards wrote. “In another, the senior leaders were resistant because they do not believe the clinical outcome should dictate the response.”
That variation of the term Just Culture is one of the limitations of the study, as those differences in implementation weren’t quantified. But in Edwards’ conclusion, he argued his findings are enough to question the value of the model.
“In the absence of proof of efficacy, hospital leaders who are committed to the pursuit of high reliability in quality and safety should be cautious about the Just Culture model,” he wrote.