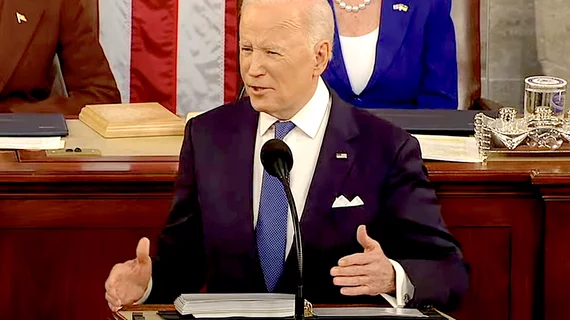
Biden signs Inflation Reduction Act into law—what does it mean for healthcare?
President Joe Biden signed the Inflation Reduction Act into law, affecting many areas across the economy, including healthcare.
The law aims to lower costs for many Americans, reduce the deficit, as well as implement climate action changes and “ask the largest corporations to pay their fair share,” according to the White House.
The act is Biden’s third major piece of legislation to sign into law since the start of his term, and it accomplishes a healthcare task the Democrats have been wanting for years: enabling Medicare to negotiate prescription drug prices. Medicare beneficiaries could also see lower prescription drug costs thanks to caps on costs included in the law and insulin caps.
Here are some of the changes in store for the healthcare space:
- Allows Medicare to negotiate prescription drug costs
- Caps pharmacy costs at $2,000 per year for Medicare Part D plans
- Insulin costs capped at $35 per month for Medicare beneficiaries
- Extension of Affordable Care Act subsidies, enabling more people to afford health insurance coverage
Many of the new healthcare implications in the law are due to begin in the coming years, with the $35 monthly cap on insulin products in Medicare Part D beginning in 2023. In 2026, Medicare will be able to negotiate with drugmakers about the prices of 10 drugs, with eligibility for 20 drugs in 2029. Plus, the Inflation Reduction Act limits the price increases of prescription drugs to below the rate of inflation, with drugmakers facing tax penalties for raising prices too high.
“The historic Inflation Reduction Act builds on the Biden-Harris Administration’s efforts to meaningfully lower healthcare costs for people across the country,” CMS Administrator Chiquita Brooks-LaSure said in a statement. “Millions of people with Medicare coverage will benefit from lower drug prices, a $35 monthly co-pay cap for insulin, a limit on out-of-pocket expenses in Medicare Part D and reduced costs under Medicare’s new ability to negotiate drug prices in the years ahead. In addition, the enhanced tax credits for the Affordable Care Act Marketplaces will continue for three years to help people afford their premiums and connect to coverage during the upcoming 10th Open Enrollment Period.”
The move to allow Medicare to negotiate drugs prices is historic and overturns the noninterference clause that was put in place in 2003 when Medicare Part D prescription drug plans were created. Medicare drug price negotiation has been promoted by healthcare associations, including the American Medical Association (AMA), for some time, as it will likely lead to lower out-of-pocket costs for beneficiaries.