EMR/EHR
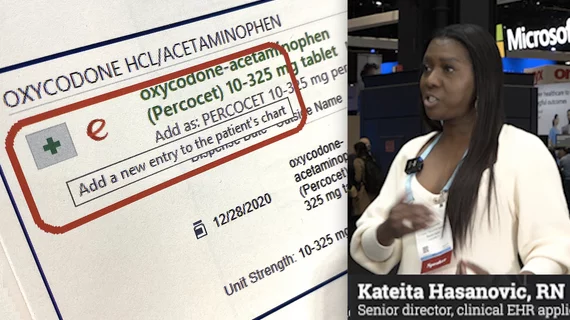
Electronic medical records (EMR) are a digital version of a patient’s chart that store their personal information, medical history and links to prior exams, texts and reports. The goal of these systems is to enable immediate access to the patient's data electronically, rather than needing to request paper file folders that might be stored in fragment files at numerous locations where a patient is seen or treated. EMRs (also called electronic health records, or EHR) improve clinician and health system efficiency by making all this data immediately available. This helps reduce repeat tests, repeat prescriptions and repeat imaging exams because reports, imaging or other patient data is not not immediately available.
Displaying 737 - 744 of 1927