Rethinking Image Sharing: Cleveland Trailblazers Link 20+ Hospitals and Provider Sites
Cleveland is yet again blazing new ground in healthcare. This time, myriad health systems are actively collaborating to share images. A first for the U.S., we believe. University Hospitals Health System (UH) is leading the charge that now includes more than two dozen hospitals, providers sites and health systems and counting. Here’s how they did it.
Watching medical-imaging CDs pour into and out of their academic medical center by the thousands every month, Beverly Rosipko and Jeffrey Sunshine, MD, PhD, knew there had to be a better way. CDs are unencrypted. They have to be transported by unpredictable human hands. They’re resource- and labor-intensive on the sending end and notoriously fussy to deal with on the receiving end. And how are the data they include best handled?
What’s worse, the list of potential snares increases exponentially when CDs—not to mention medical DVDs and/or USB drives—are getting shared not just within a large health system but between that system and other provider organizations.
Cross-institution CD fussing and shuttling was exactly what Rosipko and Sunshine wanted to curtail at 18-hospital University Hospitals Health System that stretches across 15 counties in Northeast Ohio. There, Rosipko is director of radiology informatics and Sunshine is CMIO and vice chair of radiology.
“We were often running into the issue where physicians would put a CD into a drive and find they couldn’t run it ‘for one technical reason or another,’” Rosipko recalls. “We came up with a workaround allowing our users to import the images into our PACS for temporary viewing.” But this was a Band-aid solution. “And these problems were even occurring in the OR during surgeries.”
While intent on reducing CD production and consumption, the UH imaging team wanted to do no harm to existing inter-organizational clinical collaborations. In fact, they wanted to increase cooperative image sharing, the aim being to help improve the health status of the more than 4 million people living in northeast Ohio. And they certainly knew the world was well into the age of broadband internet and cloud computing.
So it was about three years ago that the question all but asked itself among UH imaging stakeholders: Hadn’t anyone come up with a good way for ready, willing and like-minded provider institutions to go online and securely share digitized medical images?
Triple Win
Indeed someone had. It turned out to be the same technology vendor UH had selected as its PACS supplier in 2010 and for a VNA solution in 2015. The vendor is Sectra and its cloud-based Image Exchange Portal (IEP) is the solution. UH added the software in 2016. The result of the installation is image-sharing agreements with 19 area provider organizations—and counting—with UH taking a lead role driving collaborative efforts to optimize care quality and patient experience while pursuing population health and reduced costs.
The advancement in digital image-sharing “is a win-win-win,” Sunshine says. “First and foremost, it’s a win for patients and families who are trying to take care of sick loved ones. They don’t have to keep track of a CD or DVD, worrying about forgetting it or losing it or leaving it at the last doctor’s office. We’ve unburdened patients and their families.”
Second, he adds, it’s a leap forward for both the receiving and the sending provider organization. Imaging senders don’t have to burn, ship and track physical discs. Imaging receivers don’t have to deal with missing or unusable viewers, corrupted image data, potential malware exposure, digital files that just won’t open or interminable waits to see clinical images prior to the arrival of the patient bearing them.
And all three groups benefit by the avoidance of repeat imaging procedures—an unfortunately common occurrence when CDs are involved—and by the ready availability of comparison imaging for tumor staging and other critical diagnostic steps.
“It’s not often,” Sunshine says, “that we have wins across three domains.”
Collaboration on a Broad Scale
For UH, reducing CD handling also has had the happy side effect of increasing collegiality among Cleveland care providers.
During the tryout phase, one of the top attractions of the IEP was its capacity to facilitate image exchange between UH and organizations that have other cloud platforms or none at all, Sunshine and Rosipko agree. Since IEP processes data in the cloud, no one needs to install local hardware. Standard interfaces—DICOM, HL7 and XDS—handle the integration, while any of the popular web browsers will work as a password-protected entry point.
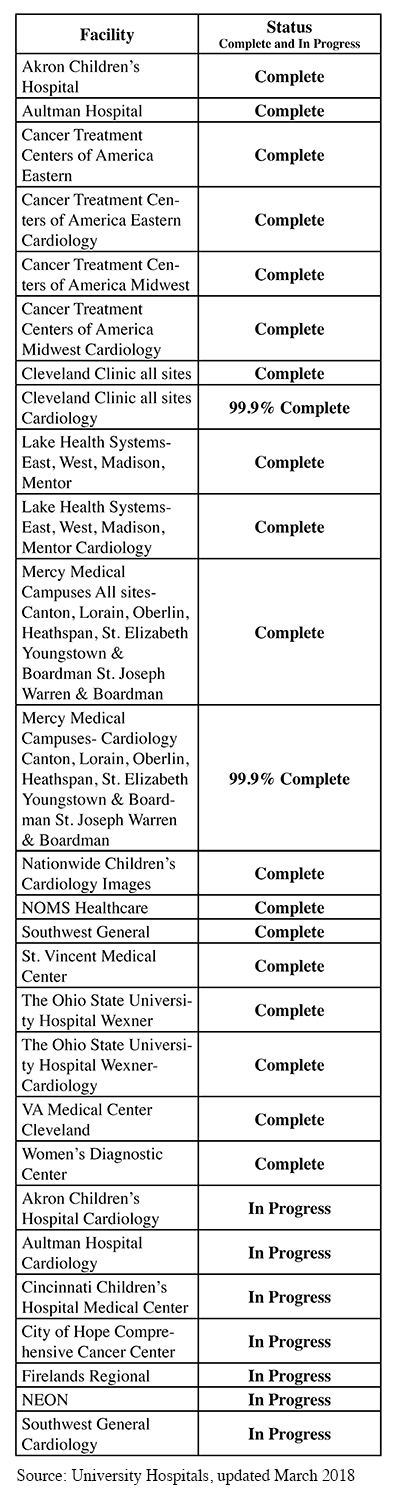
The limitless scalability of the cloud, combined with the flexibility of IEP’s onramps, has made it possible for UH to forge image-sharing relationships with provider organizations as dissimilar in size and means as the Cleveland Clinic, which has more than 4,400 beds system-wide, and 227-bed Firelands Regional Medical Center in Sandusky, Ohio. (See the list of UH’s digital image-sharing partners below.)
Image viewing can be done in more ways than one, but many end users stick with PACS and use viewers they’re familiar with. Regardless, for most, the process automatically launches in workflows that begin, as normal, in the EMR.
“I wouldn’t say that we now know everybody, but we’re certainly having more conversations than before” with image-sharing partners, Sunshine says. “University Hospital personnel talk to Cleveland Clinic people now much more than we used to,” he adds.
Hearing that, a careful observer of U.S. healthcare couldn’t help but notice that UH and the Cleveland Clinic are longtime competitors. In the age of patient-centered care, this is no small thing.
“Digital image sharing has helped to spur those conversations,” Sunshine says, “because we had to figure out how to carry it out in a cooperative way. We’re doing something that works really well for us but, more important, works really well for the patient.”
$30K-plus Instantly Saved
On the financial front, IEP’s potential as a CD buster has already translated into some impressive cost savings for UH. Rosipko cites as an example the equipment UH won’t be buying as it opens a major new ambulatory health center and freestanding emergency department in North Ridgeville, Ohio.
Right now UH has 40 or 50 CD burners, Rosipko says. There’s one at every medical center and every health center, she explains. “But we’re not buying a CD burner for North Ridgeville, and that’s saving us about $30,000 to $40,000 right there.”
She foresees a future in which UH maintains a greatly curbed fleet of CD burners, just 15 or so, and offers discs to patients and physicians who appreciate the option of having a tactile object in hand.
For UH, the long-term financial rewards of far fewer CDs in circulation could be substantial, although Rosipko acknowledges it may take some time to realize them.
“Reducing the amount of resource time to create CDs is somewhat of a wash so far, because the staff now has to be able to manage the electronic transfer,” she says. “We haven’t seen big cost savings to this point, but we expect to see significant cost savings over time, as we get more automated.”
Achieving that aim will be made easier on the staff by IEP’s intuitive interface, she continues. Upon log-in, the user immediately sees a work list detailing who has sent images or requests for images, along with relevant patient information.
“We can log into IEP and select an organization we want to request images from or send images to,” Rosipko says. “From there, we can send them the images they want or we can send them a request and they’ll get an email reading, ‘You have a request from UH for this patient’s record and the dates of the studies and types of the studies.’”
“IEP is flexible enough to accommodate just about any location that’s sending images,” she says. “If you wanted, you could give people log-in credentials so they could view the images right there in IEP. We have not done that because our physicians don’t want to have to log into a separate system. They want to see everything on the current PACS where they view clinical images today.”
Privacy and Security Assured
Along with cutting out the long waits that treating physicians had come to expect from a CD-based ecosystem for sharing images, digital image sharing assures clinicians they can be confident images are safe and secure. That’s so regardless of specialty, be it radiology, cardiology, pathology or another imaging-dependent department.
With its discrete case-by-case approval process for sending and receiving imaging data, IEP makes it inherently unattractive to cybercriminals bent on stealing health information.
“We’re not making another copy in somebody’s cloud for any substantial length of time,” says Sunshine. “We’re essentially doing PACS to PACS communication. If something nefarious happened, it would only be to one set of images—and the likelihood of that ever happening is extremely low, because nefarious people are after big repositories. We’ve avoided having a repository that could be corrupted or accessed, which is another advantage of the model we’re using here.”
Security issues accounted for, Sunshine underscores the enthusiasm with which Cleveland-area clinicians have embraced digital image sharing as a means of making their lives easier.
“The only piece that would make them even more thrilled is if there were zero delay” between request and delivery, Sunshine says. “We’re not there yet—they have to be a little bit patient waiting for approval—but we’ve done the rest.”
Into the Patient-centered Future
Sunshine is quick to credit Sectra for UH’s success leading the charge toward area-wise digital image sharing in northeast Ohio.
“To their huge credit, Sectra didn’t try to make this a side business,” he says. “We were willing to take a lead role because Sectra was willing to support IEP as a technology that they had available. There was really no significant added cost to us. That was an important piece of the puzzle.”
Both Rosipko and Sunshine look forward to seeing what could come next, including sharing non-DICOM images from throughout the enterprise and, potentially, using artificial intelligence to sift through mountains of imaging data to find relevant prior exams wherever they’re stored.
“In the near future, we’re looking toward the ability to email a link to the patient so they can receive their images electronically,” Rosipko says. “This is something we would like to be doing by the end of this year. We want to be giving our patients what they need more than ever before.”
“This technology is serving the patient,” Sunshine adds. “Digital image sharing is a way to cooperate for everyone’s benefit.”