AMA: Community practices unsustainable with low Medicare and Medicaid physician payments
Over the past decade, there has been a big increase in the consolidation of private practices into hospital systems, largely driven by reimbursement policies. Clear examples of this are include Medicare payments that cover inflationary increases for hospitals, but not for physicians—and private insurance Medicaid payments to small practices that are often below Medicare rates. The American Medical Association (AMA) said these policies impact the viability of these practices.
While current healthcare industry trends lean toward the creation of larger physician practices, the AMA said more than half of doctors still work in practices with 10 or fewer physicians. But, as payment levels continue to decline and fail to keep up with rising practice costs and inflation, some practices are facing decisions about closing their doors entirely. The AMA said this especially impacts small practices serving patients in rural, economically marginalized or underserved areas.
“While research shows that private insurance payment rates are, on average, higher than Medicare payment rates for the same medical services, it also indicates that Medicaid payment rates are substantially below Medicare payment rates. Small practices have a higher percentage of private health insurance patients than larger practices, which should benefit them. However, not all private insurance payments are reflective of the full cost of practice, the value of the care provided, or include inflation-based updates. These inadequate payment levels are exacerbated by the fact that in 2019, Medicaid fee-for-service payments for physician services were nearly 30 percent below Medicare payment levels, with an even larger differential for primary care physician services,” according to an AMA Council on Medical Service report adopted at the AMA House of Delegates 2024 meeting in June.
The report also said, while small practices have some advantages that cannot be matched by larger practices, they are not necessarily well equipped to succeed in value-based purchasing arrangements, which require financial investment and regulatory, technological and analytic expertise. “Given that the single most important factor in ensuring a sustainable level of payment for small practices is leverage, collaboration to form alliances may provide the scale needed to negotiate value-based contracts and to spread the risk across multiple practices. Strong network adequacy requirements and fair out-of-network rules are also essential for the sustainability of small practices,” the AMA report stated.
The AMA also found that the Medicare payment rate, already criticized for being too low to cover the actual costs of delivering care, is often what private insurance companies use to figure out their payment levels.
“Continuing to tether payment to a Medicare payment rate that has been reduced by almost 10% in four years presents an untenable situation for small practices,” the report says. “As such, uncoupling payment schedules from a Medicare benchmark may allow for a level of payment that reflects the full cost of practice, the value of the care provided, and includes inflation-based updates, thereby sustaining small practices.”
While it may be unfeasible to establish an equitable minimum payment rate across the six major government healthcare programs or impractical to establish a minimum payment rate in the private physician market, AMA delegates adopted policy at its June meeting stating that payment benchmarks should reflect the cost of providing care while acknowledging risk, variable expenses, an appropriate allocation of fixed costs and physician work.
Specifically, delegates called on the AMA to:
- Support making bonuses for population-based programs accessible to small community practices, without untenable exposure to administrative burden of downside risk, taking into consideration the size of the populations they manage and with a specific focus on improving care for children and maternity patients who have mental health conditions. The AMA said these groups are often disproportionately covered by Medicaid.
- Convince health insurance companies and managed care organizations to immediately uncouple their fee schedules from the Medicare physician payment schedule and maintain payment levels that are sustainable. Payments need to reflect the full cost of practice and the value of the care provided, and include an inflation-based update.
- Advocate for Children’s Health Insurance Program, Medicaid and TRICARE payments that reflect the full cost of the care provided. This includes a need for inflation-based updates, and payments at no less than 100% of the Medicare resource-based relative value scale.
Medicare physician payments trail the rate of inflation
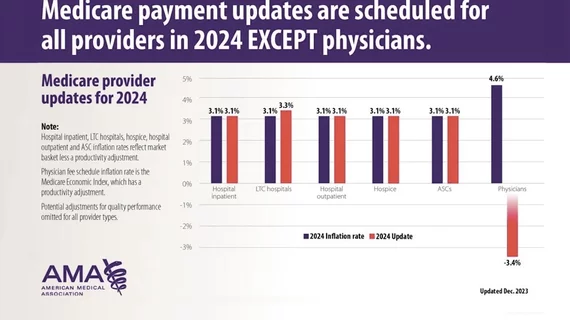
The AMA also says physicians are the only providers whose Medicare payments do not automatically receive an annual inflationary update. As a result, Medicare physician payments have lagged 26% behind the rate of inflation growth since 2001. The AMA said this statutory flaw often amplifies the impact of other payment policy changes like Medicare budget neutrality adjustments, performance incentives and others to compound lower rates to physicians.
“The AMA is deeply alarmed about the growing financial instability of the Medicare physician payment system due to a confluence of fiscal uncertainties physician practices face related to the pandemic, statutory payment cuts, lack of inflationary updates and significant administrative burdens,” the AMA said in a statement.
The association said the Medicare payment system is on an unsustainable path that will eventually result in Medicare patients being turned away because the costs to diagnose or treat them will be higher than what physicians are paid. This has been a major driver for AMA advocacy efforts in Washington to convince law makers that Medicare report is needed now to prevent issues with Medicare patient access to physicians in the near future.
The AMA and other medical societies are currently urging members to contact congressional leaders to support H.R. 2474, a bill that would modify certain adjustments to payment amounts under the Medicare physician fee schedule.
Payment amounts under the Medicare physician fee schedule are based on a service's relative value, a conversion factor, and a geographic adjustment factor. Current law provides for separate conversion factors for physicians that are qualifying participants in advanced alternative payment models (also known as qualifying APM participants) and for other physicians beginning in 2026, with an annual update of 0.75% and 0.25%, respectively. This new bill would replace the separate conversion factors for qualifying APM participants and other physicians with a single conversion factor and provides for an update that is equal to the annual percentage increase in the Medicare Economic Index, beginning in 2024.
The AMA says it is leading efforts for Medicare reform and highlights these efforts on its Fix Medicare Now website.