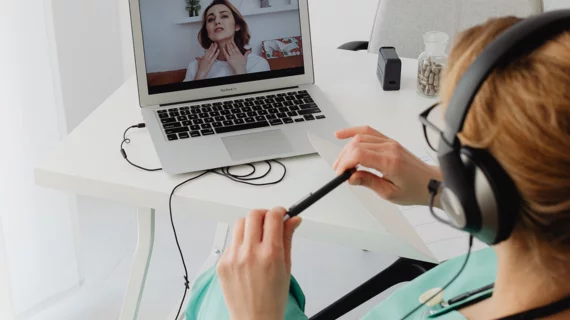
Physician plaintiff: ‘I shouldn’t have to risk losing my license—or getting jail time’ over telehealth visits
When policymakers eased rules and restrictions governing telemedicine in 2020, many patients and their doctors saw the change as one shiny silver lining in the very dark cloud that was the COVID-19 pandemic.
Unfortunately for them, the accommodation period was but a blip in time. As put by one physician lamenting the return to business as usual:
“Giving medical advice to an out-of-state patient over the phone can put me at risk of losing my license, and, in states such as California and New Jersey, of criminal charges as well.”
The physician is Shannon MacDonald, MD, a radiation oncologist at Mass General Brigham and an associate professor at Harvard Medical School.
MacDonald has taken to the pages of The Wall Street Journal to state her case for the normalization of expanded telehealth—and to illuminate the lawsuit she’s filed against the New Jersey State Board of Medical Examiners and its president, Otto Sabando, DO.
MacDonald’s co-plaintiffs in the case are University of Pittsburgh neurosurgeon Paul Gardner, MD, and some of their telehealth patients and family, including a minor.
Constitutional rights on the line
In the formal complaint, which was filed last month on the plaintiffs’ behalf by the Pacific Legal Foundation, MacDonald and fellow plaintiffs state that the U.S. Constitution’s First Amendment “prohibits the government from restricting conversations between patients and their physician-specialists based on the content of those discussions.”
Further, they assert, the Fourteenth Amendment’s Due Process Clause “does not permit the government to restrict the ability of parents to direct the medical care of their children.” More:
“Plaintiffs, who are New Jersey citizens and out-of-state specialists with patients in New Jersey, seek to vindicate their constitutional rights—and ensure they can continue to provide and receive—lifesaving care.”
Let the court settle the argument
In her WSJ commentary, MacDonald points out that securing medical licenses across state lines is so onerous that less than 1% of physicians bother to pursue interstate telemedicine.
The resulting dearth of widely available specialists reduces patient access, especially in rural areas, she notes, while solving no real-world problems.
Fees and carve-outs—for example, restricting interstate telemedicine to specialty care or requiring referrals—could head off legitimate threats and concerns like underhanded patient poaching and knotty interstate malpractice actions.
Plus teledoctors could be required to adhere to the laws of the state in which the patient is located.
“Military doctors have long been able to practice medicine across state lines,” MacDonald writes. “In 2018 it became legal for sports-team doctors to practice medicine during out-of-state away games. If we can make a law that allows treatment across state lines for a National Football League player, can’t we consider it for a child with a brain tumor?”
More:
“As a doctor, I want to provide the proper care for my patients no matter where they are, and I shouldn’t have to risk losing my license—or jail time—to do so. Because states have failed to modernize physician licensure, it’s time for the courts to weigh in.”