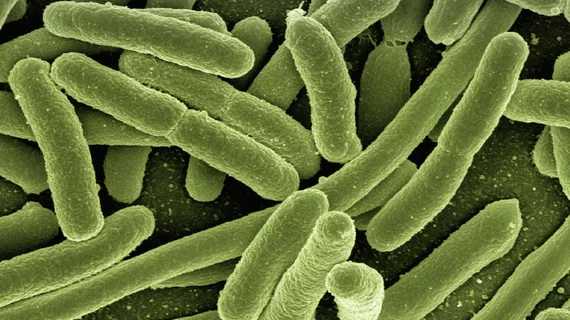
AI exposes tactics, routes taken by antibiotic-resistant infections
Horizontal gene transfer, a process by which separate organisms exchange genetic information without mating, is common among bacteria cells. It can happen directly via cell-to-cell relays or indirectly within a shared environment. Either way, along with cumulative mutations, it’s a prime facilitator of widespread resistance to antibiotic drugs.
New research shows the transfer phenomenon is predictable by machine learning. The development could help produce better weapons in the war against E. Coli and other bacterial assailants that collaborate to conquer pharmacologic first responders.
The work was carried out at Cornell University and is described online in Science Advances.
Senior researcher Ilana Brito, PhD, and colleagues applied several algorithms to a curated set of diverse bacterial genomes. The main aim was figuring out which cellular properties and functions contributed to horizontal gene transfers.
The best of their models showed genomes’ functional content predicted the transfer network with high accuracy. It achieved an area under the receiver operating characteristic curve of 0.983.
The algorithm’s performance rose higher still, to 0.990, when applied to transfers specifically involving antibiotic resistance genes.
This bounce highlighted the key role played by network structure and metabolic function in successful horizontal gene transfers, the authors comment.
From the team’s discussion section:
The predictability of recent horizontal gene transfer events provides us with a better understanding of bacterial adaptation to rapidly shifting conditions, such as those brought about by the anthropogenic dissemination of antibiotics. This opens the possibility of quantifying the risk of horizontal gene transfer between pathogens and microbiome constituents that lead to the emergence of novel antibiotic resistance strains and the expansion of reservoirs of antibiotic resistance genes within a localized context. This framework may be leveraged to improve the design of mobile genetic elements intended for engineering the microbiome or inform strategies to reduce antibiotic resistance gene burden by curing or eliminating [particular DNA fragments] or inhibiting [direct gene transfers].”
In coverage of the research by the Cornell Chronicle, Brito points out that one puzzle remains unsolved: Why do some bacteria transfer genes horizontally while others don’t?
Regardless of the answer to that question, the predictability by AI of bacterial sickness spreading via horizontal gene transfer might enable clinicians to “either intervene or choose a specific antibiotic, depending on what we see in a patient’s gut,” she says.
“More broadly, we may see where certain types of organisms are predicted to transfer with others in a certain environment. And we think there might be novel antibiotic targets in the data—for example, genes that could cripple these organisms.”