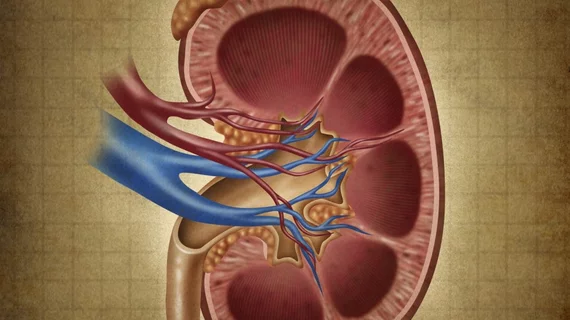
Trump administration finalizes kidney care rules
CMS has finalized changes to Medicare payment methodologies that aim to improve care for kidney care patients.
The changes to the Medicare rules affect the Durable Medical Equipment Prosthetics, Orthotics, and Supplies (DMEPOS), the End-Stage Renal Disease Prospective Payment System (PPS) and the ESRD Quality Incentive Program (QIP). There are currently more than 430,000 Medicare fee-for-service beneficiaries with end-stage renal disease (ESRD) who require about 12 hours per week on dialysis. This group of beneficiaries are among the costliest in Medicare, with the federal program spending $35.4 billion in 2016 to cover people with ESRD, and many of them have higher rates of adverse health events, such as hospitalizations
“For too long, Medicare beneficiaries suffering from kidney disease have also suffered under outdated government regulations that stand in the way of the care they need,” CMS Administrator Seema Verma said in a statement. “We are modernizing payment for durable medical equipment and advancing innovative solutions to deliver necessary treatment to those with kidney disease. This rule marks the beginning of a new era for kidney care.”
The finalized rules come after CMS proposed changes and President Trump signed an executive order in July that aimed to reduce costs and expand care options for kidney care patients. By 2030, the government aims to reduce ESRD by 30%. Medicare spends seven times more on ESRD patients compared to the average beneficiary, CMS said Oct. 31.
“Americans living with kidney disease deserve access to the latest technology that will improve their health, and HHS is proud to be delivering that as part of our actions under President Trump’s executive order,” HHS Secretary Alex Azar said in a statement. “Payment reforms are just part of a holistic effort HHS is undertaking, including through public-private partnerships like KidneyX, to support the next generation of kidney health technologies.”
The changes offer payment adjustments that recognize the costs of new therapies, which means certain new and innovative equipment and supplies for an ESRD patient qill qualify for a transitional add-on payment adjustment. CMS also made changes to payment for new kidney-related drugs, but the agency is still refining those adjustments, it said. Within DMEPOS, Medicare payment for new items will be based on commercial pricing data.
See the final rule here.