5 things to know about state health system performance rankings
The Commonwealth Fund’s 2018 scorecard on state health system performance saw the five highest-ranked states maintain their exact rankings from the last report, with Hawaii again claiming the No. 1 spot. The most striking finding was the surge in deaths from suicide, alcohol and overdoses from opioids and other drugs since 2005.
“Overall, healthcare quality and access have improved for people since the major coverage expansions of the Affordable Care Act took effect,” said David Radley, PhD, MPH, senior scientist for The Commonwealth Fund's Tracking Health System Performance program and lead author of the report. “But these gains are at risk as premature deaths from treatable diseases and opioid overdoses rise across the country. We need to ensure that every community has a strong primary care system, including integrated mental health services, so that we can address these growing gaps in life expectancy.”
The rankings are based on 43 measures ranging from uninsured rates to 30-day hospital mortality to potentially avoidable emergency department visits. Here are five key findings of the report:
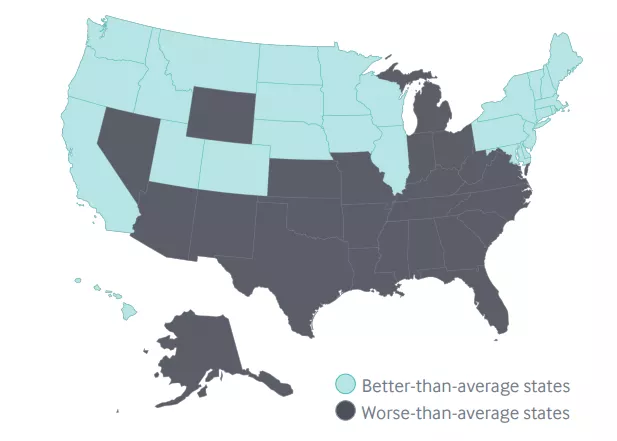
1. Which states are up, which are down, which are improving
The top five states overall were unchanged from the previous report: Hawaii took the top spot, followed by Massachusetts, Minnesota, Vermont and Utah. At the bottom, Mississippi was again at No. 51 (the District of Columbia is included in the scorecard), with Oklahoma at No. 50 trailing Louisiana, Florida and Arkansas.
Some of those lower-ranked states actually saw some of the biggest improvement since the last report. Arkansas, Louisiana and Oklahoma each improved on 17 indicators in the study. New York saw the greatest improvement, boosting scores on 18 indicators, included decreases in elderly patients being prescribed high-risk drugs and hospital admissions for ambulatory care-sensitive conditions among Medicare beneficiaries.
Radley and his coauthors credit several state-level healthcare policies for New York’s improvement, such as creating a state-based insurance exchange under the Affordable Care Act and implement a Delivery System Reform Incentive Program (DSRIP) for its Medicaid population.
2. “Deaths of despair” on the rise
The combined death rates for these so-called “deaths of despair” increased by 50 percent between 2005 to 2016. Rates were higher in all states over that time and in five—Delaware, Ohio, New Hampshire, New York and West Virginia—is the increase was at least twofold.
West Virginia, a state hit hard by the opioid epidemic, had the worst score on this measure, with 83.1 deaths per 100,000 population.
At the same time, the report found “pervasive” gaps in care for mental health. 56 percent of adults with mental illness and 18 percent of children with those needs receiving no treatment.
“Reversing these trends and closing gaps in care will likely require cooperation across sectors as well as greater integration of medical, behavioral, public health, and social services,” the report said.
Radley and his coauthors also found several quality measures presenting pressing challenges for states as life expectancy has actually decreased in recent years. Deaths from preventable or treatable causes increased in two-thirds of states between 2014 and 2015, with six states—Colorado, Maine, Nebraska, Oklahoma, Vermont and Wyoming—reporting an increase of higher than 5 percent.
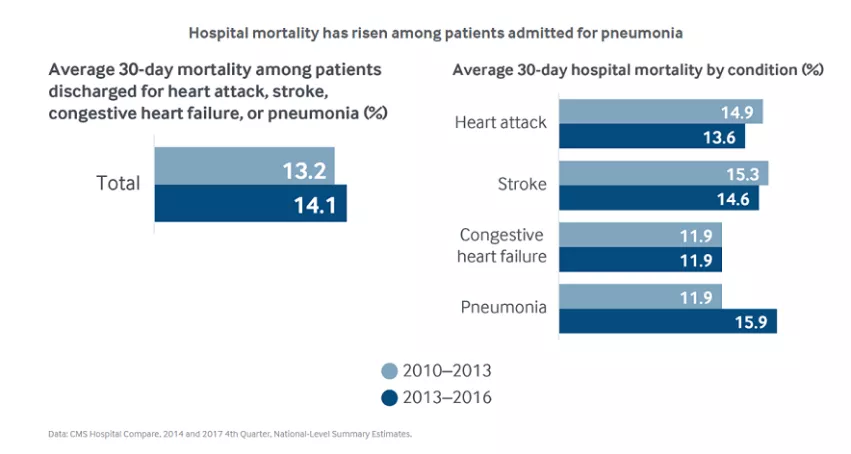
3. Hospital mortality increasing
The report include measures of death within 30 days of Medicare beneficiaries’ hospital discharge for four common conditions: heart attack, strike, congestive heart failure and pneumonia. The combined rate rose in nearly every state between the 2013 to 2013 and 2013 to 2016 measurement periods, with the national average jumping from 13.2 to 14.1 percent.
When broken down by condition, the increase appeared to be entirely driven by pneumonia mortality.
4. Higher spending doesn’t equal better care
The U.S. as a whole has been shown to have higher healthcare spending than other states without having better outcomes. That same finding trickles down to the state level with quality “not in line” with levels of state spending which exceed the median per capita spending in 10 other high-income countries.
While access to care and insurance coverage have increased since the passage of the Affordable Care Act, the report found persistent gaps in quality. For example, 29 percent of working-age adults with employer-sponsored insurance and who were newly diagnosed with lower back pain in 2015 received potentially unnecessary imaging tests. In Alabama, the worst-performing state in this category, the number reached 41 percent.
5. Improvements in nursing home and home health
Some of the bright spots in the report were centered on measures for nursing home and home health patients. Radley and his coauthors found a decline in nearly all states on the use of antipsychotics as “chemical restraints” for nursing home residents. For home health patients, the share who reported improved ability to walk or move around rose “substantially” across the country.