ML’s Role in Building Confidence and Value in Breast Imaging
Countless predictions have been made about artificial intelligence and machine learning changing imaging screening and diagnosis at the point of patient care—and clinical studies and experience are now proving it. Radiologists say the impact is real in improving diagnosis of cancers and quality of care, consistency among readers and reducing read times and unnecessary biopsies. One shining example targets the evaluation of breast ultrasound imaging.
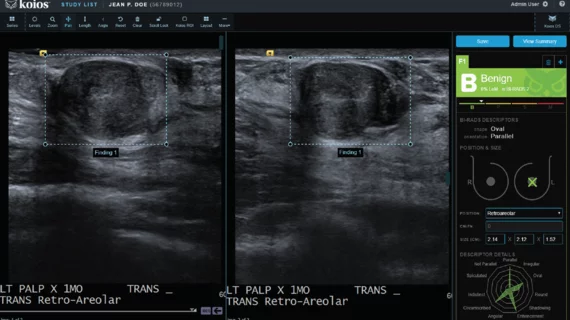
Main Street Radiology in the New York City borough of Queens has been using machine learning software to analyze breast ultrasound images for screening and diagnosis for almost a year. The software, Koios DS for breast from Koios Medical, helps radiologists come to fast and accurate assessments of lesion characteristics and BI-RADS assessments. Hardware-agnostic, the software is compatible with most PACS.
“What’s great about the software is that it allows for lesions that do not conform to an exact shape, such as an oval shape with one or two microlobulations,” or bumps on the margins, explains Lai Yu, MD, co-section chief for breast imaging at 40-physician Main Street Radiology in Queens. “It allows us to have the confidence to make the call as to whether it’s really something worrisome or not.”
Viewing the image on a monitor, the radiologist drags an icon over the lesion of interest. The algorithm—which has been trained on hundreds of thousands of breast-lesion images—presents recommendations for lesion characteristics as well as a preliminary BI-RADS assessment. The tool is “very simple,” says Yu, who is also a clinical assistant professor of radiology at Weill Cornell Medical College of Cornell University. “You look at it and right away you basically know how to use it. Finding something easy to use is the key to what a good AI program is.”
Clinical studies prove the ML algorithm enhances diagnosis. A study in the Journal of Digital Imaging demonstrated an upcoming version of Koios DS for breast improved accuracy in breast cancer diagnosis for all radiologists across all levels of experience which is note-worthy because research shows physicians interpret the same cases differently, in up to one of every three cases. Sensitivity increased from a range of 92 to 97 percent to a range of 97 to 98 percent, and specificity increased from a range of 38 to 46 percent to a range of 45 to 52 percent. Benign biopsy rates were reduced 25 to 55 percent without a reduction in sensitivity.
A similar study published in 2017 in Cancer Research found a cancer identification rate of 100 percent with a 69 percent reduction in benign biopsies.
Yu took a closer look with her colleagues too, examining 100 cases sent to pathology. “It was sobering but made it very obvious to us that machine intelligence helps us as radiologists when we realized we could possibly have avoided 40 biopsies,” she says. “It can help us do a better job.”
CATCHING MORE CANCERS
For breast radiologists, getting better means catching more true cancers while reducing false positives and uncertain diagnoses. The latter can be both stressful and unnecessarily risky for patients, as receiving a diagnosis designated “tentative” often means undergoing a biopsy, returning (or staying) for more imaging—or both.
As for AI in healthcare as a whole, radiology is a natural early AI adopter. Medical images are a perfect fit for applying the same ML techniques that the Department of Defense uses to recognize human faces.
The front lines in the war against breast cancer are a perfect place to launch ML directly into patient care. According to the American Cancer Society, breast cancer is the second leading cause of cancer death in women behind lung cancer. Yet, thanks largely to early detection in screening due to heightened public awareness, death rates from female breast cancer dropped 39 percent from 1989 to 2015.
At Main Street Radiology, Yu says she uses ML in about 15 percent of the cases she reads. That may sound low, but it’s “quite impactful,” she says, “because those are the cases where you’re scratching your head. Having that second opinion for those kinds of cases makes a big difference.”
IT’S ALL ABOUT THE PATIENT
Yu also is focused on enhancing the patient experience—and increasing value in the patient care process. In fact, the literature is already beginning to bear this out.
In December 2018, two physicians from the University of California, Davis, published an analysis in the American Journal of Roentgenology concluding that AI technologies can, paradoxically, help radiologists demonstrate their value in the domain of the human touch.
“The promise of AI is its potential to release physicians from tasks that are better performed by automation,” wrote Radiologist Shadi Aminololama-Shakeri, MD, and Cardiologist Javier E. López, MD. “AI may enhance our diagnostic accuracy to the point that we are able to refocus on the art of the doctor-patient relationship.”
It is all about the patient, Yu agrees. “The yield of this may not be obvious until you realize that you’re recommending fewer biopsies and short-term follow-ups for findings that are benign,” she says. “Those things in and of themselves represent significant improvements in a practice. Administrators have to realize that your yield is not concrete. But having radiologists be so much more accurate—and better—in itself is worth it.”
Watch Expert Roundtable with Q&A - Architecting AI: Why Machine Learning Is Changing Medical Imaging
-
View more features from this issue:
Building Foundations to Build Better Care
Embracing AI: Why Now Is the Time for Medical Imaging
Leveraging Technology, Data and Patient Care: How Geisinger Is Interjecting Insight & Action
Bullish on AI: The Wisconsin Way: Reengineering Imaging & Image Strategy
Will ‘Smart’ Solutions Really Transform Cardiology?
Matching Machine Learning and Medical Imaging: Predictions for 2019
NYU’s Daniel Sodickson on AI, Facebook and Why Faster MR Scans Could Improve Healthcare