FDA has now cleared more than 500 healthcare AI algorithms
(An updated version this article was posted December 2023 - FDA has now cleared 700 AI healthcare algorithms, more than 76% in radiology)
There are now more than 520 market-cleared artificial intelligence (AI) medical algorithms available in the United States, according to the U.S. Food and Drug Administration (FDA) as of January 2023. The vast majority of these are related to medical imaging.
Here is the breakdown for the number of FDA-cleared algorithms across specialties:
• Radiology 396
• Cardiology 58
• Hematology 14
• Neurology 10
• Clinical chemistry 7
• Ophthalmic 7
• Gastroenterology and urology 5
• General and plastic surgery 5
• Pathology 4
• Microbiology 4
• Anesthesiology 4
• General Hospital 3
• Orthopedic 1
• Dental 1
See the complete list of FDA-cleared algorithms here
The first AI algorithm was cleared by the FDA in 1995, and fewer than 50 algorithms were approved over the next 18 years. However, the numbers have increased rapidly in the past decade, and more than half of algorithms on the U.S. market were cleared between 2019 to 2022––more than 300 apps in just four years. Last October, the FDA approved 178 new AI and machine learning (ML) systems. That number is expected to grow rapidly into the future, the FDA has said.
AI and ML technologies have the potential to transform healthcare by deriving new and important insights from the vast amount of data generated during the delivery of healthcare every day. Medical device manufacturers are using these technologies to innovate their products to better assist healthcare providers and improve patient care, the FDA explained on its website.
Medical imaging makes up the majority of FDA-cleared AI algorithms
"Artificial intelligence is really good at discerning patterns within the data. There has been a lot of work in the medical imaging space, where AI can really help improve diagnostic capabilities with image recognition," explained Julius Bogdan, an AI expert and vice president and general manager of the Healthcare Information and Management Systems Society (HIMSS) Digital Health Advisory Team for North America.
HIMSS sees the movement toward wider AI adoption as one of the biggest trends in healthcare information technology (IT). The clinical side of AI requires regulatory clearance, and the majority FDA-approved algorithms are imaging related across subspecialties.
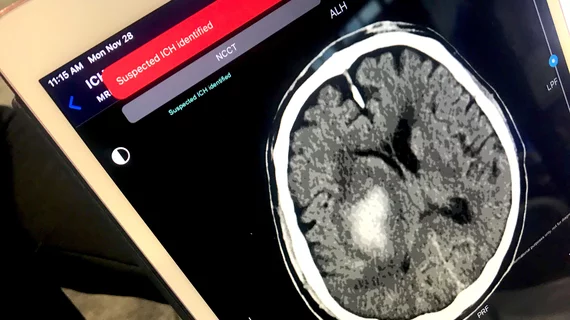
AI's high accuracy of pattern recognition has led to a concentration of market approvals on the imaging side. AI can be trained using thousands or tens of thousands in images that show the various presentations of a specific disease, such as ischemic and and hemorrhagic stroke, specific cancers, breast density or coronary shift plaque morphology. Most of the radiology applications focus on specific subspecialty imaging, such as brain, breast, cardiac, lung and stroke imaging.
Not surprisingly, several of the cardiology, ophthalmic, surgical, obstetrics/gynecology, gastroenterology and urology, dental and pathology AI systems also involve medical imaging.
"Today, we live in that quadrant of things humans can do and humans are supervising," explained Keith J. Dreyer, DO, PhD, FACR, American College of Radiology (ACR) Data Science Institute chief science officer. Dreyer also holds the positions of vice chairman of radiology at Massachusetts General Hospital, chief data science and information officer for the departments of radiology for both Massachusetts General Hospital and Brigham and Women's Hospital
"That is all the FDA-approved AI stuff that we see today," Dreyer said. "Even though all these FDA-approved algorithms are using AI, it is not all what most people think of, where it is making a diagnosis or finding a lesion. There is a big variety in the ways to classify AI."
The areas of AI in imaging include:
• Diagnostic aids that can automatically identify critical findings.
• Automation of time-consuming functions such as quantification, contouring and auto complete of text in reports.
• Workflow improvements and automation.
• Data mining applications.
• Clinical decision support for next steps in the patient's care or to ensure imaging exam meets the guidelines.
• Modality specific AI to iso-center patients, choosing imaging protocols, or speeding MRI exam time.
• AI to enhance image reconstructions, to improve image quality, resolution, and identify and fix imaging artifacts.
• Guidance AI to help imagers get the best possible images, even if they are novice users of the system or are unfamiliar with the anatomy.
• Automatic anatomical identification, labeling and contouring of organs or specific types of tissue.
AI expanding into non-clinical areas of healthcare
AI algorithms do not require FDA clearance if they do not directly impact clinical care, and this type of use is also seeing rapid proliferation across healthcare.
Non-clinical AI is often used in IT systems to sort through the vast amounts of patient data to pull out relevant pieces of information for specific patient encounters, Bogdan said. It's also used to search for population health traits. This data can target some patients for additional care or resources, streamline diagnosis or workflow or aid in data mining or identifying patterns in data, which can be very difficult for humans to do easily.
"With the advent of the modern electronic health record (EHR), healthcare became more of a data industry, and the analytics of that data has begun to play or more prominent role across healthcare," Bogdan explained. "AI has started to gain some momentum in healthcare in a lot of different areas."
This trend is clearly evident at the annual HIMSS meetings, where AI messaging is seen everywhere across the vast expo floor of more than 1,400 vendors.
Bogdan explained several key areas where non-clinical AI is being implemented in healthcare:
• Population health
• Health tracking apps
• Identifying and addressing gaps in health equity
• Revenue cycle management streamlining
• Hospital-wide monitoring for length of stay, bed turn over rates, early sepsis detection and readmissions
• Data analytics for key performance indicators
• Enabling better patient wellness and preventative care
A growing number of companies and health systems are now using health tracking apps to better monitor patients' health. According to Bogdan, this is another area where AI can help, namely by monitoring large amounts of patient data and identifying people who may require physical followup, or those who may have issues with mental health or burnout.
"There is a growing body of research that is being incorporated into these health and wellness applications, and AI is at the heart of a lot of them. That might include how to de-stress or offering information about nutrition, suggesting medical tests you may need or a list of medical providers you can see," Bogdan explained.
FDA looking at changing its regulatory approach to AI
AI products are different from previous types of software, since some types of AI can learn on their own once deployed. The FDA requires a new approach to how the cleared AI algorithms are monitored over time once they are in real-world healthcare settings.
When reviewing AI products, the FDA’s Center for Devices and Radiological Health (CDRH) is considering a total product lifecycle-based regulatory framework for these technologies that would allow for modifications to be made from real-world learning and adaptation, while ensuring that the safety and effectiveness of the software as a medical device are maintained. Such a regulatory framework could enable the FDA and manufacturers to evaluate and monitor a software product from its premarket development to post-market performance. This approach could allow for the FDA’s regulatory oversight to embrace the iterative improvement power of AI and ML-based software as a medical device, while assuring patient safety. This system under consideration is based on feedback from a 2019 AI stakeholder's meeting, and the proposed framework is outlined in a 2021 action plan.