FDA approves new Alzheimer’s disease drug
The U.S. Food and Drug Administration (FDA) has approved a new drug treatment for Alzheimer’s disease, Leqembi (lecanemab).
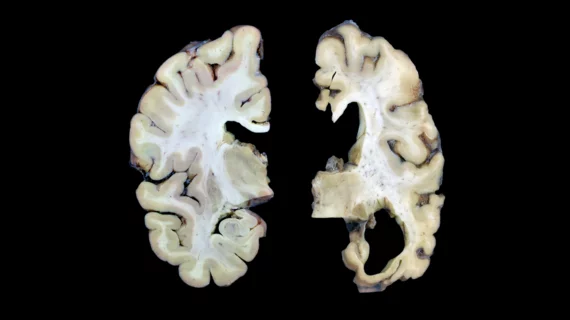
The approval of the drug, which was granted with the agency's Accelerated Approval pathway, was met with excitement within the healthcare industry due to its potential impact on the Alzheimer’s population. An estimated 6.5 million Americans age 65 and older were living with Alzheimer’s disease in 2022, according to the Alzheimer’s Association. The disease is an irreversible, progressive brain disorder that slowly destroys memory and thinking skills, the FDA stated.
Leqembi, developed by Japanese pharmaceutical company Eisai, is based on the observed reduction of amyloid beta plaque, a marker of Alzheimer’s disease.
“Alzheimer’s disease immeasurably incapacitates the lives of those who suffer from it and has devastating effects on their loved ones,” said Billy Dunn, MD, director of the Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research. “This treatment option is the latest therapy to target and affect the underlying disease process of Alzheimer’s, instead of only treating the symptoms of the disease.”
The Global Alzheimer’s Platform Foundation voiced its support for the approval and excitement for its potential to impact people with Alzheimer’s. The foundation also urged the Centers for Medicare and Medicaid Services (CMS) to offer the treatment to patients as soon as possible.
“Lecanemab significantly lowers amyloid plaque buildup in the brain, which means that people on this therapy have a better chance of maintaining a good quality of life. After reviewing the data, the FDA has clearly identified the clinical benefit, supporting the use of lecanemab as a safe and effective treatment—a life-sustaining treatment—for people living with Alzheimer’s disease,” said Global Alzheimer’s Platform Foundation President John Dwyer. “With this approval, it is incumbent on Center for Medicare and Medicaid Services (CMS) Administrator Chiquita Brooks-LaSure and the drug’s sponsors to offer this life-changing therapy to patients quickly, while prioritizing access and economic fairness.”
CMS stated the Accelerated Approval of the drug treatment falls under its existing national coverage determination, and if lecanemab subsequently receives traditional FDA approval, CMS would provide broader coverage. The Accelerated Approval pathway allows the FDA to “approve drugs for serious conditions where there is an unmet medical need and a drug is shown to have an effect on a surrogate endpoint that is reasonably likely to predict a clinical benefit to patients,” the agency said.
The FDA approved the drug treatment after the results of a Phase 3 randomized, controlled clinical trial confirmed the drug's clinical benefit. In a study of 856 patients with Alzheimer’s disease was conducted with patients receiving the approved dose of lecanemab, 10 milligram/kilogram every two weeks. Patients receiving the drug showed “a statistically significant reduction in brain amyloid plaque from baseline to Week 79 compared to the placebo arm, which had no reduction of amyloid beta plaque,” the FDA said.
The drug treatment does carry some risk of brain swelling “that usually resolves over time and may be accompanied by small spots of bleeding in or on the surface of the brain, though some people may have symptoms such as headache, confusion, dizziness, vision changes, nausea and seizure,” the FDA stated.
The drug will be co-marketed with Biogen, a U.S.-based pharma manufacturer that has collaborated with Eisai for nearly a decade.
"The approval of Leqembi provides new hope to patients with Alzheimer's disease. Patients at an early stage of the disease and their caregivers can now consider a new treatment option with their doctors. Our focus now is on the path forward, working alongside Eisai with the goal of making Leqembi available to patients who may benefit from this treatment as soon as possible," Christopher A. Viehbacher, president and CEO of Biogen, said in a statement.